Abstract
Introduction:
The PETAL trial is a multicenter randomized controlled study for patients with aggressive lymphomas of diverse histologies (EudraCT 2006-001641-33, NCT00554164). In patients with diffuse large B-cell lymphoma (DLBCL) interim PET (iPET) reliably predicted progression-free survival (PFS) and overall survival (OS). Interim PET-based treatment changes had no impact on outcome (ASH 2014, abstract 391; ASH 2016, abstract 1857). To further improve outcome prediction we developed a new dynamic scoring system combining baseline total metabolic tumor volume (TMTV) with age and early iPET response.
Methods:
TMTV was measured in 510 patients with newly diagnosed DLBCL participating in the PETAL trial. Patients aged 18 to 80 years with a positive baseline PET received 2 cycles of rituximab (R), cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) followed by iPET and randomisation. In total, patients received 6 or 8 cycles of standard R-CHOP or 2 cycles of R-CHOP followed by 6 cycles of an intensive protocol originally designed for the treatment of Burkitt's lymphoma. A favorable iPET was defined as a reduction of the maximum SUV by > 66% compared to baseline. By using the 41% maximum standardized uptake value (SUV41max) thresholding method, baseline TMTV was calculated. Cut-off values were determined by receiver operating characteristic (ROC) analysis. The Youden index was used to compute the optimal cut-off point. Kaplan-Meier survival analysis was performed to estimate PFS and OS. By using uni- and multivariate cox-regression prognostic factors were analyzed.
Results:
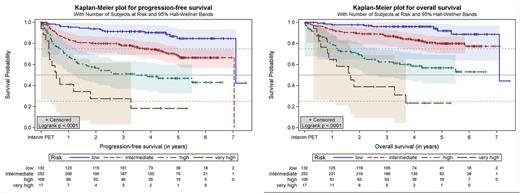
Median follow-up was 4.4 years. The optimal cut-off for baseline TMTV was identified to be 313 cm3 with 310 patients (60.8%) belonging to the low TMTV group (range, 0.91-306.24 cm3) and 200 patients (39.2 %) belonging to the high TMTV group (319.71-8895.88cm3). A low baseline TMTV (< 313 cm3) was associated with a significantly better 5-year PFS (77.1% vs. 50.2%, p < 0.0001) and 5-year OS (84.1% vs. 64.3%, p < 0.0001). By creating a new prognostic score based on age (> 60 years =1 point), baseline TMTV (≥ 313 cm3 =1 point) and early iPET response (unfavorable =1 point) we identified four different risk groups: low (0 points) with a 5-year PFS of 84.6% (95% confidence interval [CI] 74.5% - 90.9%) and a 5-year OS of 91.9% (CI 82.3% - 96.4%), intermediate (1 point) with a 5-year PFS of 68.5% (CI 61.3% - 74.6%, p = 0.0003, hazard ratio [HR] 2.78) and a 5-year OS of 79.8% (CI 73.5%-84.8%, p = 0.0054, HR 2.78), high (2 points) with a 5-year PFS of 46.8% (CI 36.5%-56.5%, p < 0.0001, HR 6.31) and a 5-year OS of 56.7% (CI 45.9%-66.2%, p < 0.0001, HR 8.15) and very high (3 points) with a 5-year PFS of 18.3% (CI 3.7%-41.8%, p < 0.0001, HR 14.91) and a 5-year OS of 23.3% (CI 6.2%-46.7%, p < 0.0001, HR 18.75).
Conclusion:
Baseline TMTV is highly predictive for outcome in patients with DLBCL. By combining baseline TMTV with age and early iPET response we developed a new and easy to apply PET-based scoring system that detects patients at high and very high risk of disease progression and early death. Compared to the International Prognostic Index [IPI] and the enhanced NCCN-IPI the new score provided much better separation of curves.
Hüttmann: Bristol-Myers Squibb, Takeda, Celgene, Roche: Honoraria; Gilead, Amgen: Other: Travel cost.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal